Understanding the Vital Importance of Accurate Temperature Measurement in South Africa's Healthcare System
Effective Temperature Monitoring as a Cornerstone for Achieving Optimal Health Outcomes
Accurate body temperature monitoring is fundamental in the sphere of healthcare, especially in the diverse climatic landscape of South Africa. The country's varying climatic conditions, ranging from the warmth of coastal zones to the chill of elevated highlands, necessitate careful monitoring. Elevated body temperatures can signal serious health issues, such as infections, requiring prompt medical attention. Given the varied demographics and ecological zones across South Africa, precise temperature measurement is essential. For instance, in high-altitude areas like the Drakensberg, individuals may display different baseline temperatures due to environmental influences. Recognising and adapting to this variability is crucial for accurate health evaluations and effective treatment strategies. Therefore, mastering precise temperature measurement and interpretation is vital for the successful management of health in South Africa's multifaceted population.
In-Depth Exploration of Temperature Measurement Techniques Commonly Used in South Africa
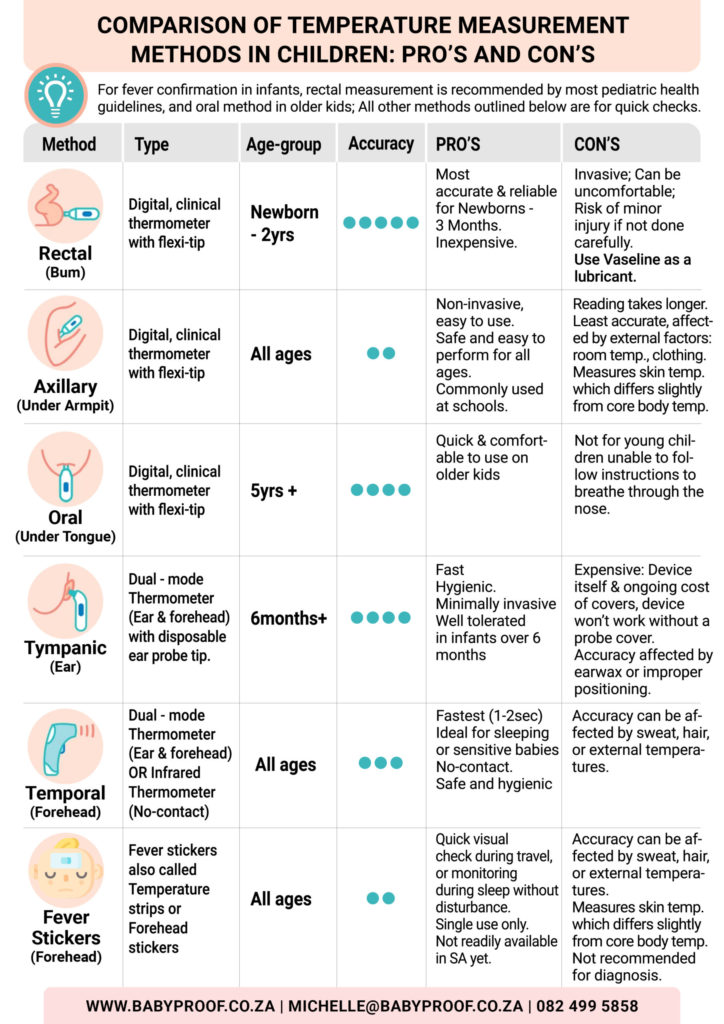
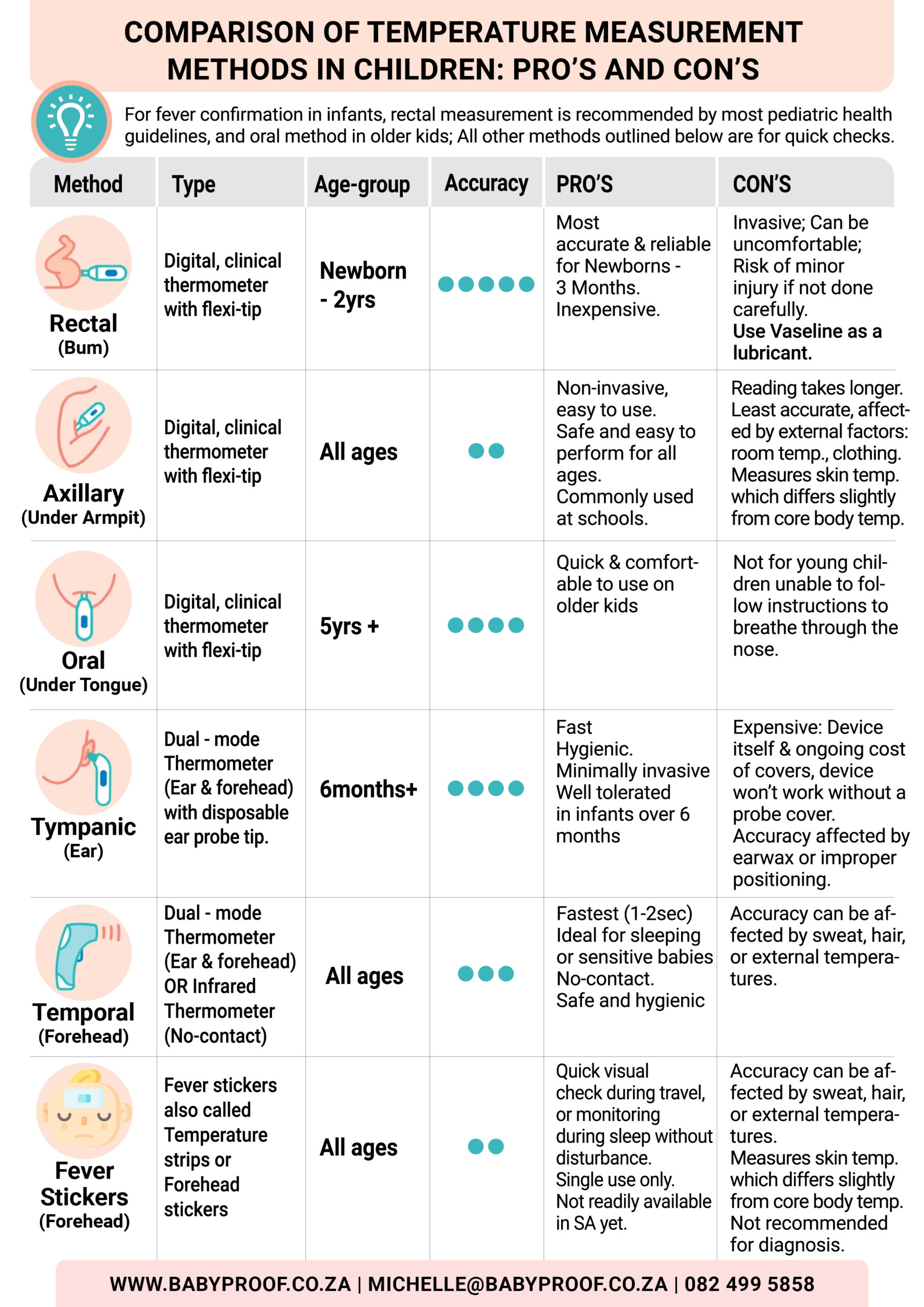
In South Africa, common methods for measuring body temperature encompass oral, axillary, and rectal techniques, each possessing distinct advantages and practical considerations tailored to various situations. Oral thermometers are widely available in homes and medical facilities, providing a reliable balance of convenience and accuracy. Although axillary measurements are often utilised in schools and childcare settings due to their non-invasive nature, they are usually regarded as less precise. Conversely, rectal measurements, while less frequently employed outside clinical environments, are considered the gold standard for precision, particularly for vulnerable populations like infants or critically ill patients. Familiarity with these measurement techniques and their appropriate applications is essential for effective health monitoring throughout South Africa, ensuring that healthcare providers can make informed decisions based on accurate readings.
Best Practices for Temperature Measurement Techniques Across Various Age Groups in South Africa
- Newborn – 3 months → Opt for Rectal (most reliable) or Temporal (forehead) for swift and efficient screening.
- 3 months – 3 years → Rectal for accuracy; Temporal (forehead) or Axillary (underarm) for greater comfort.
- 4 – 5 years → Oral if the child can cooperate; Temporal (forehead), Tympanic (ear), and Axillary (underarm) for rapid assessments. Consider using Fever Stickers as an alternative.
- 6+ years → Oral for the best combination of accuracy and comfort; Temporal (forehead) or Tympanic (ear) for quick evaluations.
CLICK HERE TO DOWNLOAD FREE PRINTABLE COPY
The Significant Influence of Accurate Temperature Readings on Patient Health Outcomes
Obtaining precise temperature readings is crucial for diagnosing illnesses and monitoring health effectively, particularly in a nation like South Africa, where diverse environmental conditions can markedly affect physiological responses. In clinical settings, healthcare professionals depend heavily on accurate temperature measurements to inform their treatment decisions. For instance, an inaccurately recorded temperature could lead to unnecessary treatments or delays in addressing critical health issues. Moreover, in community health initiatives, ensuring accurate temperature readings can substantially improve the effectiveness of public health responses, particularly during disease outbreaks. Therefore, the importance of accuracy in temperature measurement cannot be overstated, as it has a direct impact on patient outcomes and overall public health.
Understanding the Effects of Altitude on the Accuracy of Temperature Measurements
The diverse altitudes present in South Africa pose unique challenges for temperature measurement. Locations such as <a href=”https://limitsofstrategy.com/bryanston-golf-club-a-tranquil-escape-in-johannesburg/”>Johannesburg</a>, which lies approximately 1,753 metres above sea level, may show variations in body temperature readings when compared to coastal cities like Durban. Increased altitude can lead to alterations in body metabolism and thermoregulation, requiring careful adjustments in interpreting temperature readings. Healthcare providers must take these variations into account when assessing patients from different regions. For instance, a fever in a patient from a high-altitude area may present differently compared to someone from a lower elevation. Recognising these subtleties is essential for accurate health evaluations and tailored patient care.
Recent Technological Innovations in Temperature Monitoring Equipment
In recent years, South Africa has witnessed significant technological advancements that have improved the efficiency and accuracy of temperature monitoring. Innovations such as infrared thermometers and digital devices are increasingly being adopted in both clinical and home settings. These advanced devices provide rapid temperature readings and often include user-friendly features, such as backlit displays and memory functions. Additionally, the emergence of smartphone-connected thermometers has gained traction, allowing users to track their temperature readings over time and easily share this data with healthcare providers. These technological advancements not only streamline the temperature measurement process but also have the potential to enhance health outcomes by facilitating timely medical interventions.
Mastering the Techniques for Accurate Oral Temperature Measurement in South Africa
A Step-by-Step Process for Accurately Taking an Oral Temperature Reading
Taking an oral temperature reading is a straightforward procedure that requires placing the thermometer under the tongue while ensuring that the mouth remains closed for an accurate measurement. It is crucial to verify that the patient has not consumed any hot or cold foods or beverages at least 15 minutes prior to taking the reading, as these factors can significantly impact the results. Once the thermometer is properly positioned, one should wait for the device to signal that the reading is complete, typically indicated by an audible beep. Educating patients and caregivers on this technique is essential to ensure that it is performed correctly, reducing the risk of inaccurate readings. This method is commonly utilised in South African households, making it accessible for family members to conveniently monitor their health.
The Advantages of Oral Temperature Measurement Techniques
Oral temperature measurement offers numerous advantages that make it the preferred choice in various South African households and healthcare environments. Firstly, this method is non-invasive, significantly reducing discomfort often associated with alternative temperature-taking techniques. Secondly, it is user-friendly, allowing individuals to take readings without requiring professional assistance. This convenience makes it particularly suitable for quick checks at home, where families can effortlessly monitor fevers in both children and adults. Additionally, oral thermometers typically provide quick results, generally within one to two minutes, facilitating prompt health decisions. In South Africa's fast-paced environments, this efficiency is especially beneficial for families needing rapid health assessments.
Understanding the Limitations and Considerations of Oral Temperature Measurement
While oral temperature measurement has numerous advantages, it is not without its limitations. This method may not be suitable for all patient demographics, particularly young children or individuals who cannot hold the thermometer in place for the required duration. Furthermore, factors such as recent food or drink consumption, smoking, or even breathing through the mouth can influence the accuracy of readings. In South Africa, where environmental conditions can vary widely, outdoor temperatures can also affect readings if the thermometer is not used correctly. Therefore, when employing the oral method, it is critical to consider these factors to achieve the most accurate results possible, ensuring reliable health monitoring.
Delving into Axillary Temperature Measurement Techniques in South Africa
Proper Techniques for Measuring Temperature Using the Axillary Method
The axillary method entails positioning the thermometer in the armpit and ensuring that the arm is pressed snugly against the body for an accurate reading. This technique is widely employed in South African schools and childcare facilities due to its safety and ease of performance for individuals of all ages. It is essential to ensure that the skin is dry and that the thermometer is correctly placed to achieve optimal accuracy. The reading may require a longer duration than oral methods, often taking several minutes. Educating caregivers and staff on the proper technique is vital to ensure that temperature readings are reliable and effective for identifying health concerns in both children and adults.
The Benefits of Using Axillary Temperature Measurement Techniques
Axillary temperature measurement presents several benefits, particularly in public health settings throughout South Africa. One of the main advantages is its non-invasive nature, making it safe for individuals of all ages, including infants and the elderly. The ease of performing this method allows for quick execution in school health programmes or health fairs, where time constraints may be present. Additionally, the axillary approach is cost-effective, requiring fewer resources compared to advanced digital or infrared thermometers. This accessibility is particularly important in rural areas, where healthcare resources may be limited. The simplicity and safety of axillary measurements make them an excellent option for community health initiatives, promoting effective health monitoring.
Factors That Can Impact the Accuracy of Axillary Temperature Measurements
Despite its advantages, various factors can affect the accuracy of temperature readings obtained through the axillary method. Environmental conditions, such as high ambient temperatures or humidity levels prevalent in South Africa, may lead to elevated readings due to perspiration, potentially indicating a false fever. Furthermore, clothing can create insulation, hindering heat exchange and distorting results. Movement during the measurement process, particularly in children, can also lead to inaccurate readings. Therefore, healthcare providers and caregivers must be aware of these factors and implement measures to mitigate their impact, such as ensuring the arm remains close to the body and that the skin is dry before conducting measurements.
Exploring Rectal Temperature Measurement Techniques in South Africa
How to Accurately Measure Rectal Temperature with Confidence
Accurately measuring rectal temperature involves several careful steps to ensure both precision and patient comfort. First, it is essential to apply lubricant to the tip of the thermometer to facilitate gentle insertion. The thermometer should be inserted approximately an inch into the rectum while being held securely, waiting for the reading to complete. This method is frequently employed in South African hospitals due to its precision, particularly in critical care scenarios or when monitoring infants. Given its sensitivity, performing the process gently and with the patient’s comfort in mind is essential to maintain trust and cooperation from patients, especially those who are vulnerable.
Why Rectal Temperature Measurement is Considered the Most Accurate
Rectal temperature measurements yield the most accurate readings compared to oral and axillary methods, making them ideal for critical care situations in South Africa. This accuracy is particularly crucial in emergency contexts or when dealing with unresponsive patients, as healthcare professionals rely on precise temperature information to guide treatment decisions. Additionally, rectal thermometers are less susceptible to external variables, such as ambient temperature or recent oral intake, rendering them a reliable option in clinical practice. In paediatric care, especially for infants, rectal measurements provide a definitive assessment of core body temperature, enabling timely and appropriate medical responses crucial for patient safety.
Important Considerations and Precautions for the Rectal Measurement Method
Despite its advantages, the rectal measurement method necessitates certain considerations and precautions. The insertion process can be uncomfortable, potentially leading to patient resistance, particularly in non-clinical settings. Therefore, it is vital to clearly explain the procedure and reassure the patient to foster cooperation. Furthermore, healthcare providers must adhere to strict hygiene protocols to prevent any potential infections or injuries. Due to these concerns, rectal measurements are less frequently performed in home settings across South Africa. Nonetheless, understanding when and how to utilise this method is critical for healthcare professionals to ensure the utmost care and accuracy in temperature monitoring, safeguarding patient well-being.
Expert Guidance on Choosing the Most Suitable Temperature Measurement Method
Insights from South African Health Experts on Temperature Measurement Practices
Health professionals in South Africa often recommend various temperature measurement methods based on several factors, including the patient's age, health condition, and specific context. For example, oral measurements are typically suggested for adults and older children who can securely hold the thermometer. Conversely, axillary readings might be preferred for quick assessments in schools or community health screenings. Rectal measurements are generally advised for infants or critically ill patients due to their accuracy. Below are some expert recommendations:
- For adults: Prefer oral or rectal readings for enhanced accuracy.
- For young children: Use axillary or rectal methods based on cooperation levels.
- For infants: Rectal measurements are the gold standard for precision.
- In school settings: Axillary readings are often adequate for quick health checks.
- In emergencies: Prioritise rectal measurements for accurate assessments.
These recommendations underscore the importance of selecting the temperature measurement method tailored to the individual needs of each patient and the context in which care is provided, ensuring optimal health outcomes.
Understanding the Influence of Environmental Conditions on Temperature Readings in South Africa
Environmental factors in South Africa significantly impact temperature readings, necessitating that healthcare providers consider the context while interpreting data. For instance, in coastal locations where humidity levels are elevated, axillary temperature readings may be artificially raised due to excessive sweating, potentially leading to misdiagnosis. Similarly, in colder regions, such as the Drakensberg, ambient temperatures can cause a drop in readings, prompting healthcare professionals to remain vigilant about local conditions. Experts advocate that practitioners adjust their interpretation of temperature data based on these environmental variables, ensuring accurate assessments. This contextual awareness is crucial for appropriate diagnosis and treatment, ultimately improving patient care.
Implementing Best Practices for Temperature Measurement in South Africa
Implementing best practices for temperature measurement is vital in South Africa to ensure accurate and reliable readings. These practices include regularly calibrating thermometers to maintain their precision, as poorly calibrated devices can yield misleading results. Moreover, healthcare providers should understand patient conditions and adapt their temperature measurement techniques accordingly. For example, considering a patient’s hydration status can significantly influence readings. Providers should also educate patients and caregivers about the importance of using proper measurement techniques, including the timing of readings and understanding factors that may affect temperature. By adhering to these best practices, healthcare professionals can significantly enhance the quality of care delivered throughout South Africa.
Cultural Beliefs and Their Impact on Temperature Measurement Preferences in South Africa
Cultural beliefs play a significant role in shaping temperature measurement preferences in South Africa. Various communities may favour specific methods based on traditional practices or comfort levels. For instance, some cultures might prefer non-invasive methods like axillary measurements due to a preference for less intrusive techniques. Acknowledging these cultural nuances is essential for healthcare providers to deliver culturally sensitive care. Engaging with communities to educate them about the benefits and limitations of each temperature measurement method can build trust and improve adherence to recommended practices. Furthermore, respecting cultural beliefs while offering evidence-based recommendations can enhance patient cooperation and health outcomes.
Challenges in Implementing Various Temperature Measurement Methods in South African Healthcare Facilities
Implementing temperature measurement methods in South African health facilities presents various challenges, including resource availability and staff training. In rural areas, healthcare facilities may lack access to modern temperature-taking devices, limiting effective monitoring. Additionally, staff may require continuous education and training to ensure they are proficient in accurately using various measurement methods. High patient volumes in urban clinics can also lead to time constraints, resulting in rushed assessments and potential inaccuracies. Addressing these challenges through targeted training programmes and improving equipment access is crucial for enhancing temperature monitoring practices throughout South Africa's diverse healthcare landscape.
Comparative Insights on Oral, Axillary, and Rectal Temperature Measurement Methods
Key Differences Between Temperature Measurement Techniques
The key differences between oral, axillary, and rectal temperature measurement techniques primarily centre around accuracy, ease of use, and suitability for various age groups and settings. Oral thermometers provide reliable readings and are frequently used for adults and older children. However, they necessitate patient cooperation, which may not always be feasible. Axillary temperature measurements are non-invasive and suitable for all ages, making them ideal for community screenings; however, they tend to be less precise. Rectal measurements, often regarded as the most accurate, may cause discomfort and might not suit all patients outside clinical environments. Understanding these distinctions is essential for selecting the most appropriate method for each specific situation, ensuring effective health monitoring.
Evaluating Accuracy and Reliability Across Temperature Measurement Methods
In South Africa, the accuracy and reliability of temperature readings differ across the various methods. Rectal measurements are generally recognised as the most accurate, closely reflecting core body temperature. Oral measurements follow, yielding reliable readings when performed correctly, while axillary measurements typically result in the least accurate outcomes. This hierarchy of accuracy guides healthcare providers in their choices, especially when assessing febrile patients or making critical care decisions. For instance, in emergency settings, rectal readings may be prioritised to ensure precise monitoring of patients' conditions. Acknowledging the limitations of each method can significantly enhance healthcare quality in South Africa, ultimately leading to better patient outcomes.
Suitability of Each Temperature Measurement Method in South African Contexts
The appropriateness of each temperature measurement method within South African contexts depends on various factors, such as the setting and the patient's specific needs. In home environments, oral measurements are often favoured for older children and adults due to their convenience. In contrast, axillary measurements may be standard in schools or during community health campaigns, where quick assessments are necessary. Rectal measurements, while ideal for precise monitoring in clinical settings, may be less suitable for home use due to comfort concerns. Therefore, healthcare providers must carefully evaluate each situation, considering available resources and the patient's condition to determine the most suitable temperature measurement method, ensuring effective patient care.
Practical Considerations for Effective Temperature Measurement in South Africa
Available Equipment and Resources for Temperature Measurement Across South Africa
The range of equipment and resources for temperature measurement in South Africa varies significantly. From basic digital thermometers to advanced clinical devices, the options available are extensive. In urban hospitals, cutting-edge technology is often utilised, including infrared thermometers that allow for rapid and contactless measurements. Conversely, in rural settings, basic thermometers may be the only option, which can affect the accuracy of readings. The availability and affordability of these tools greatly influence healthcare practitioners’ choice of methods across the country. Ensuring that healthcare facilities, particularly in underserved areas, have access to reliable equipment is crucial for effective patient care and accurate health assessments.
Challenges Faced in Temperature Measurement Practices
Healthcare providers in South Africa encounter numerous challenges regarding temperature measurement. Limited resources, especially in rural regions, can restrict access to accurate and reliable thermometers. Moreover, patient cooperation can be unpredictable, particularly in children or individuals with cognitive impairments, making accurate measurement difficult. Unique environmental factors, such as extreme heat or cold, can also interfere with readings and complicate assessments. Overcoming these challenges involves employing strategies such as community education initiatives, improving equipment access, and training healthcare providers on best practices for temperature measurement to enhance health monitoring across the country.
Strategies to Ensure Accurate Temperature Readings in South Africa
Achieving accurate temperature readings in South Africa involves several critical steps. First, healthcare providers should consistently evaluate their techniques to ensure adherence to best practices for each measurement method. Regular calibration of thermometers is also essential for maintaining accuracy. Educating patients and caregivers about the significance of proper technique, including factors that can influence readings, such as recent food intake or environmental temperature, can greatly enhance assessment reliability. Practitioners should also consider the distinct environmental conditions of South Africa to appropriately adjust their interpretation of readings, ensuring comprehensive patient care and effective health outcomes.
Reliable Strategies for Selecting the Best Temperature Measurement Method
Determining the Most Effective Temperature Measurement Method for South Africans
Selecting the best method for temperature measurement in South Africa requires thoughtful consideration of several factors. First, the patient's age and health condition significantly influence the appropriate method. For example, infants may necessitate rectal measurements for accuracy, while older children might be more suited to oral or axillary methods. Additionally, the setting—whether in a clinical environment, at home, or during a community health event—should guide the choice of measurement. South Africans can adopt these strategies to ensure informed decision-making:
- Assess the patient’s age and level of cooperation.
- Consider the urgency of the temperature assessment.
- Evaluate available equipment and resources.
- Be aware of environmental conditions that may affect readings.
By following these steps, individuals can ensure they select a method that delivers reliable results, leading to informed health decisions.
Best Practices for Each Temperature Measurement Method in South Africa
Implementing best practices for temperature measurement is critical across all methods used in South Africa. For oral measurements, always confirm that the patient has not consumed anything that could affect readings beforehand. When performing axillary measurements, keeping the arm close to the body and ensuring the skin is dry will yield more accurate results. Rectal measurements require careful handling and clear communication with the patient to minimise discomfort. Best practices for each method include:
- Regularly calibrate thermometers to ensure accurate readings.
- Educate patients and caregivers on proper techniques.
- Consider environmental factors when interpreting results.
- Document findings accurately to facilitate ongoing health assessments.
Following these practices will enhance the reliability of temperature measurements and improve health outcomes throughout South Africa, ensuring that patients receive the best possible care.
Strategies for Educating the South African Public on Temperature Measurement
Public education on temperature measurement is essential for enhancing health literacy across South Africa. Healthcare providers can establish clear guidelines that outline the importance of accurate temperature readings and how to measure them effectively. Community outreach programmes, workshops, and health fairs can serve as platforms to educate the public about various temperature measurement methods. Moreover, utilising local healthcare resources, such as clinics and hospitals, to disseminate information and provide demonstrations can improve understanding. By focusing on practical application and cultural relevance, healthcare professionals can foster a more informed public capable of effectively monitoring their health.
Assessing Best Practices for Temperature Measurement in South Africa
Key Insights on Temperature Measurement Practices
Oral, axillary, and rectal temperature measurement methods each possess distinct advantages and limitations within South African healthcare. Understanding the unique characteristics of each method, including accuracy, ease of use, and age appropriateness, is crucial for effective health monitoring. By being aware of the environmental factors that can influence readings, healthcare professionals can make informed decisions that enhance patient care and contribute to improved health outcomes.
Recommendations for Healthcare Providers in South Africa
Healthcare providers in South Africa should consider individual patient needs, including age and health status, when selecting temperature measurement methods. Furthermore, they should remain cognizant of available resources and the environmental context to ensure accurate assessments. Ongoing training and education on the latest best practices will further empower providers to deliver high-quality care in temperature monitoring, leading to better health outcomes for patients across the nation.
Emerging Trends in Temperature Measurement Practices in South Africa
Future trends in temperature measurement may include the adoption of advanced technologies, such as smart thermometers that connect to mobile applications for tracking health metrics. Enhanced public education initiatives can further elevate health literacy regarding temperature measurement. Additionally, tailored approaches that consider South Africa's unique cultural and environmental contexts will improve the effectiveness of healthcare delivery in temperature monitoring, ensuring that all individuals receive the care they need.
Disparities Between Rural and Urban Settings in Temperature Measurement Practices
The choice of temperature measurement methods may differ dramatically between rural and urban settings in South Africa. Limited access to advanced equipment in rural areas may necessitate reliance on simpler methods like axillary readings. In contrast, urban facilities often have access to a wider array of technological options, permitting more precise measurements. Addressing these disparities through targeted resource allocation and training is vital to ensure equitable healthcare access across the nation, improving health outcomes for all.
The Influence of Cultural Practices on Temperature Measurement Preferences in South Africa
Cultural beliefs and practices significantly shape attitudes towards temperature measurement methods in South Africa. Understanding and respecting these beliefs is imperative for healthcare providers to deliver culturally sensitive care. By engaging with community leaders and incorporating culturally relevant practices into health education, providers can ensure that temperature measurement methods are accepted and effectively utilised within various cultural contexts. This approach fosters trust and improves adherence to recommended health practices, ultimately benefiting patient care.
Frequently Asked Questions About Temperature Measurement Techniques
Which method is considered the most accurate for measuring body temperature?
The rectal method is widely regarded as the most accurate for measuring body temperature, as it closely reflects core body temperature and is less influenced by external factors.
Can axillary temperature be relied upon for accurate diagnosis?
While axillary temperature is non-invasive and safe, it is generally less accurate than oral or rectal methods. However, it can still provide useful information in non-critical settings.
What is the correct procedure for taking an oral temperature reading?
To take an oral temperature, place the thermometer under the tongue, close the mouth, and wait for it to beep. Ensure that no hot or cold food or drink has been consumed beforehand, as this can affect the reading.
What factors can compromise the accuracy of axillary temperature readings?
Factors such as ambient temperature, humidity, clothing, perspiration, and movement can all influence the accuracy of axillary temperature readings, leading to potential misinterpretations.
Is it safe to measure rectal temperature in a home setting?
While rectal measurements are accurate, they can be uncomfortable. They are generally recommended for infants or in clinical settings rather than at home unless advised by a healthcare professional.
What technologies are available for temperature measurement in South Africa?
In South Africa, a variety of technologies is available, ranging from basic digital thermometers to advanced infrared devices that enable quick, non-contact temperature measurements, enhancing convenience and accuracy.
How frequently should thermometers be calibrated?
Thermometers should be calibrated regularly to ensure accuracy, ideally before significant use each season or at least once a year, to maintain their reliability.
What actions should I take if my temperature reading is abnormal?
If a temperature reading is abnormal, especially if accompanied by other symptoms, it is advisable to seek medical advice for further evaluation and potential treatment.
Are there cultural preferences for temperature measurement methods in South Africa?
Yes, cultural beliefs can impact preferences for specific temperature measurement methods. Understanding these beliefs is vital for providing culturally sensitive healthcare, ensuring that patients feel respected and comfortable.
How can I learn more about temperature measurement techniques?
You can learn more about temperature measurement techniques through local healthcare providers, community health workshops, and online resources dedicated to health education, enhancing your understanding.
Check out our vibes on Instagram!
The article Best Method for Temperature: Oral, Axillary, or Rectal? A South African Guide was published first on: https://www.babyproof.co.za
The Article Temperature Measurement Methods: Oral, Axillary, or Rectal? Was Found On https://limitsofstrategy.com
The Article Temperature Measurement Methods: Oral, Axillary and Rectal Options found first on https://electroquench.com